Time: 2024-07-29
A groundbreaking study from Tulane University has uncovered a potential new treatment that may help eliminate HIV from one of its most stubborn hiding places - the brain . The research , published in the journal Brain , shows that an experimental drug originally developed for cancer treatment significantly reduced levels of SIV , the nonhuman primate equivalent of HIV , in the brains of infected animals . Lead study author Woong - Ki Kim , PhD , associate director for research at Tulane National Primate Research Center , explains the significance of this breakthrough in managing HIV - related brain issues.
While current antiretroviral therapy ( ART ) has transformed HIV from a terminal illness to a manageable condition , it falls short of completely eradicating the virus . HIV persists in viral reservoirs in the brain , liver , and lymph nodes , where it remains out of reach of ART . The brain has been particularly challenging due to the blood - brain barrier , which protects the organ from harmful substances but also blocks treatments . This persistence of HIV in the brain is believed to contribute to neurocognitive dysfunction , experienced by nearly half of those living with HIV.
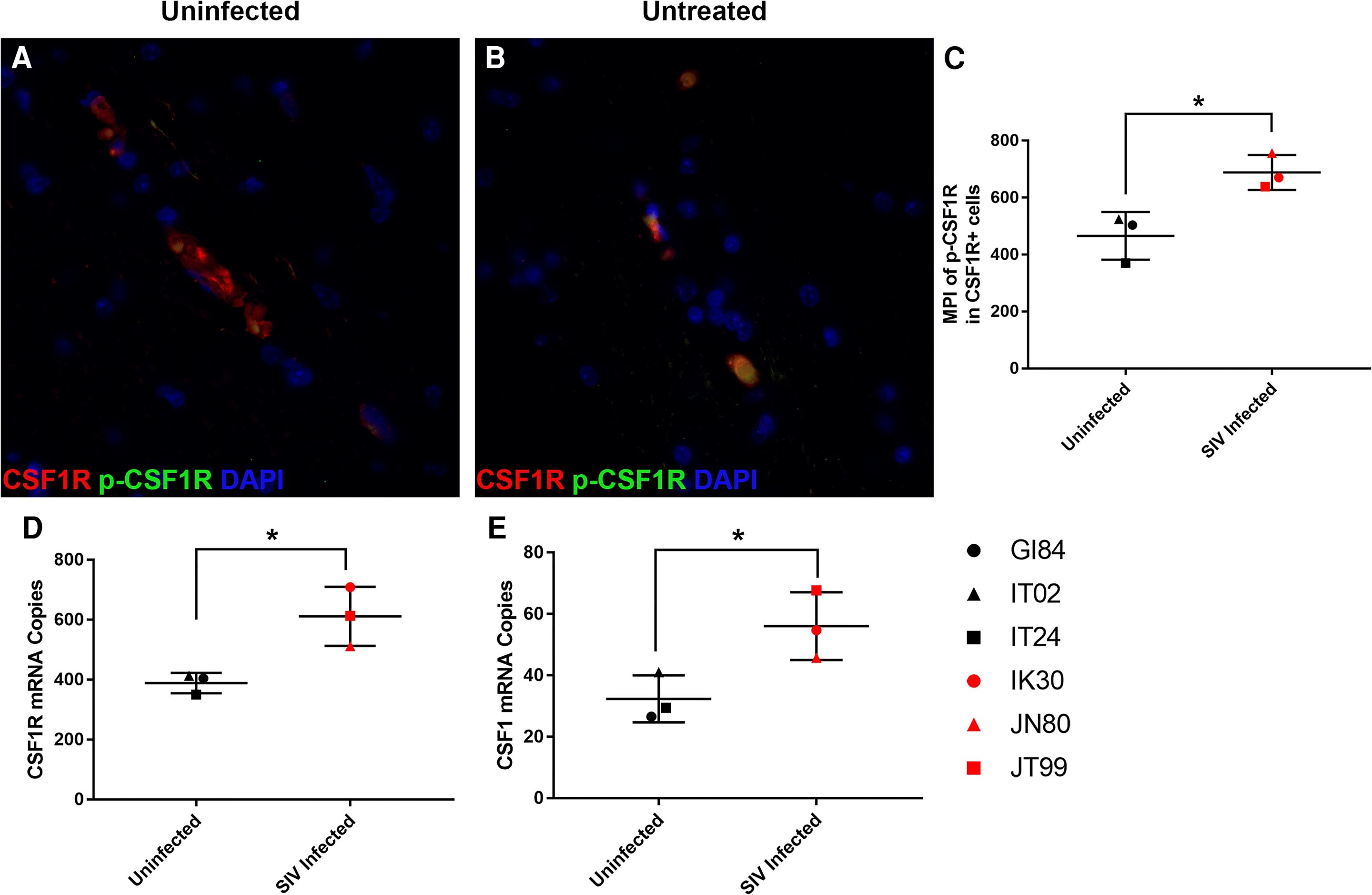
The Tulane team focused on macrophages , a type of white blood cell that harbors HIV in the brain , using a small molecule inhibitor called BLZ945 to block a receptor that increases in HIV - infected macrophages . The study , conducted at the Tulane National Primate Research Center , used three groups to model human HIV infection and treatment : an untreated control group , and two groups treated with either a low or high dose of BLZ945 for 30 days . The high - dose treatment led to a remarkable 95 - 99 % decrease in viral DNA loads in the brain without impacting microglia , the brain 's resident immune cells crucial for maintaining a healthy neuroimmune environment.
This groundbreaking research opens up new possibilities for managing HIV / AIDS by targeting infected brain cells . The small molecule inhibitor BLZ945 , originally developed for cancer treatment , has shown promising results in reducing viral loads in the brain . While the study is still in its early stages , the next step is to test this therapy in conjunction with ART to assess its efficacy in a combined treatment approach . This could lead to more comprehensive strategies for eradicating HIV from the body entirely and potentially improving cognitive outcomes for those living with HIV.
As research progresses , the impact of this discovery extends beyond HIV treatment . The approach of targeting specific cells in the brain could potentially be applied to other neurological conditions where certain cell types play a key role in disease progression . Funded by the National Institutes of Health , this study offers hope for more effective treatments and even a possible cure for HIV in the future , marking a significant step forward in HIV research.